Photodamage: Preventing Sun-Induced Aging
Explore the use of antioxidant shields, lifestyle practices, SPF strategies, and the power of Mitopure® to protect skin against photodamage.

What to know
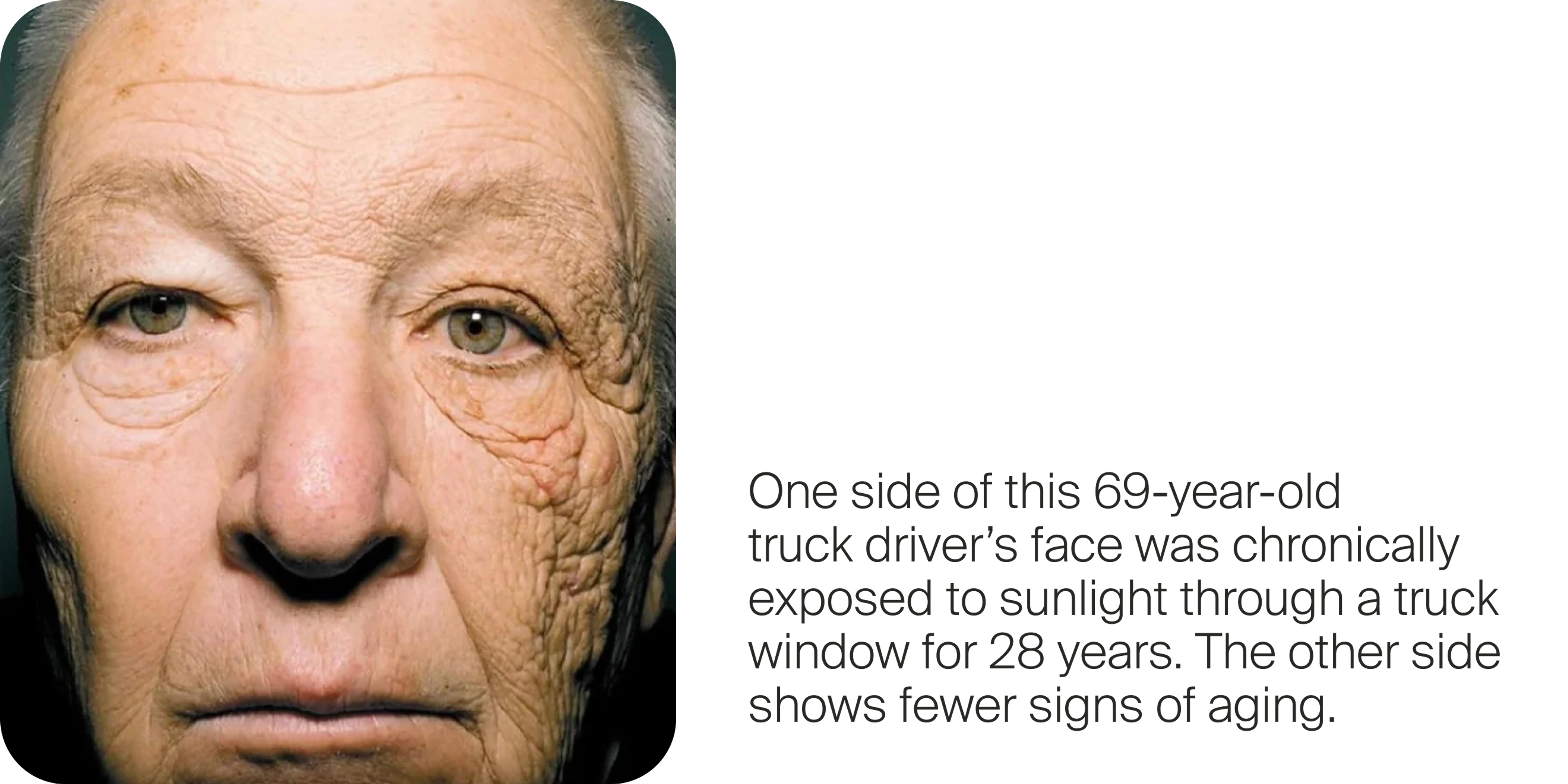
Photodamaged skin accounts for up to 80% of visible aging, but it’s largely preventable with daily protection and smart skincare.
UV and visible light penetrate skin, damaging DNA, collagen, and mitochondria, accelerating the aging process.
Skin sensitivity to photodamage varies widely, but no one is immune; sun protection matters for all skin tones.
Topical Mitopure® promotes a significantly milder sunburn response, without sensitizing or irritating the skin.
Photodamaged Skin: How to Protect and Prevent Sun-Induced Aging
The sun is life-giving; without it, none of us would be here. It warms us, feeds our plants, and even helps our bodies make vitamin D. So you might wonder, how can something so essential also be so harmful to our skin?

Why We Need SPF More Than Ever
While basking in the sun feels good, wearing SPF is more essential than ever. Decades ago, we could enjoy the sun with a much lower risk of skin damage, but today, things have changed. There are several reasons for this.
One key reason is the thinning of the ozone layer. This protective shield in our atmosphere plays a crucial role in filtering out harmful ultraviolet (UV) radiation. Chemicals and pollution from our industrial lifestyle have thinned the ozone layer, and as it becomes depleted, more UV rays reach the Earth’s surface, increasing the potential for skin cell damage with prolonged sun exposure.[1]
Additionally, our diets are not as rich in antioxidants as they once were. Nutrients like vitamin C and E, polyphenols, omega-3 fatty acids, and beta carotene can help to protect our skin from the inside out. As a population, we are eating fewer foods rich in these nutrients. The result is less natural resilience against high-energy light.
What Is Photodamaged Skin?
Photodamage, also known as sun damage, refers to the harm caused to the skin by exposure to ultraviolet (UV) radiation. These UV rays penetrate the skin, causing damage to:
- DNA, leading to mutations and increased cancer risk[2]
- Collagen and elastin, causing wrinkles and sagging[3]
- Mitochondria, reducing the skin's ability to repair itself[4]
- Skin cells, generating harmful free radicals and inflammation[5]
Photodamage accelerates aging skin, and it’s been reported that it is the leading cause of premature skin aging, accounting for up to 80% of visible aging signs.[7] And, it contributes to the risk of developing skin cancer. With predictions that 1 in 5 Americans will get skin cancer in their lifetime, this is a serious concern.[6]
The good news? It’s largely preventable.
What Are The Signs of Photoaging?
Common signs of photoaging include:
- Wrinkles: These wrinkles tend to be more pronounced than the fine lines of biological aging.[8]
- Discoloration: Uneven skin tone with hyperpigmented spots (ie, sun spots), as well as areas of mottled pigmentation.[9]
- Visible veins. You may notice redness or broken capillaries (spider veins) on the nose, cheeks, and neck.[10]
- Texture changes: Photoaged skin can become rough, dry, or thickened with a leathery appearance, and may develop a sallowness.[11]
- Loss of elasticity: Sun damage degrades collagen and elastin in the skin, leading to sagging or lax skin.[12]
A damaged skin barrier has more difficulty locking moisture in and keeping pathogens out. This can also lead to irritation, sensitization, and inflammation.[13]
What Causes Photoaging and Photodamage?
What causes photoaging? In a word: light.
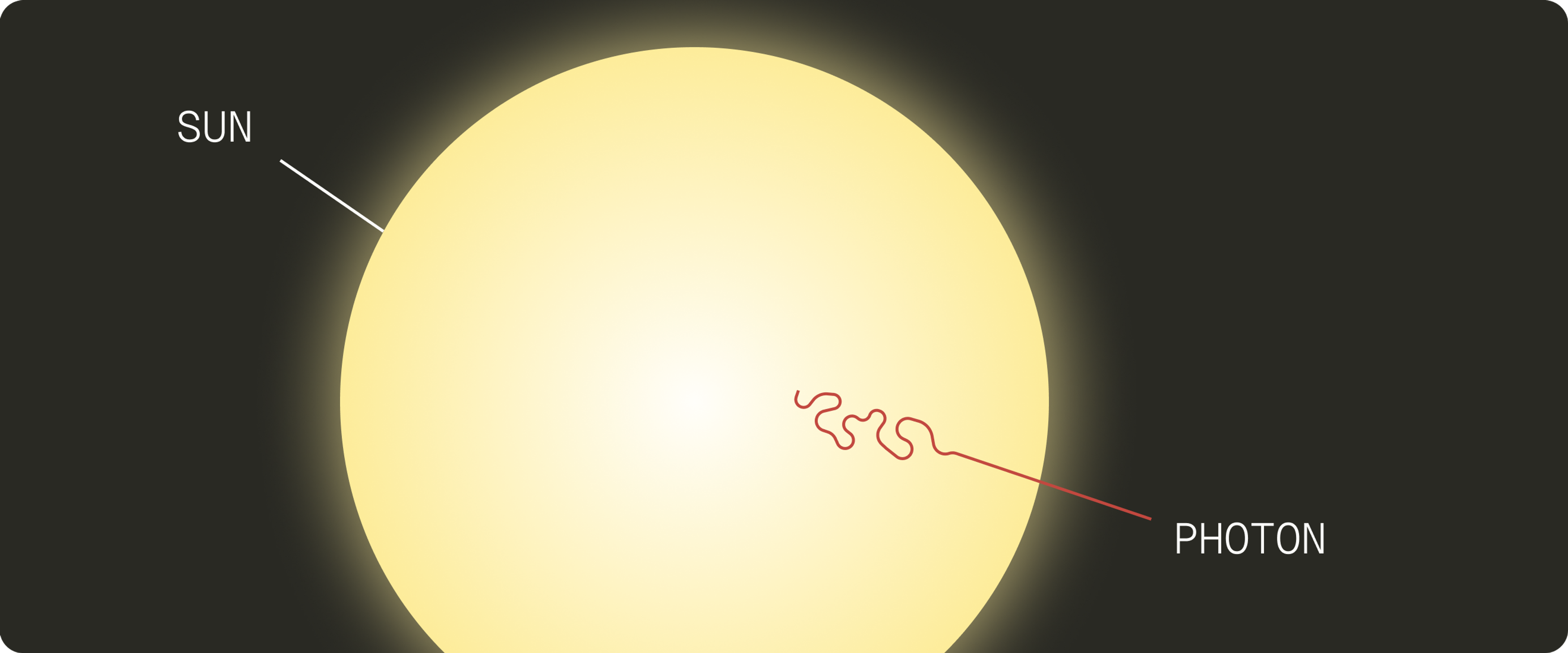
Light particles (i.e., photons) are very high energy, both literally and metaphorically. When we’re exposed to sunlight or visible light, some of the photons bounce off our skin, while others penetrate.[14]
The photons that get into your skin are like uninvited guests at a house party. Their high energy rubs off on nearby atoms, and suddenly your quiet get-together is a total rager.
The result is atomic chaos: bonds break, molecules get damaged, free radicals are born, and your skin’s structural integrity begins to erode[15].
Photodamage and Mitochondria
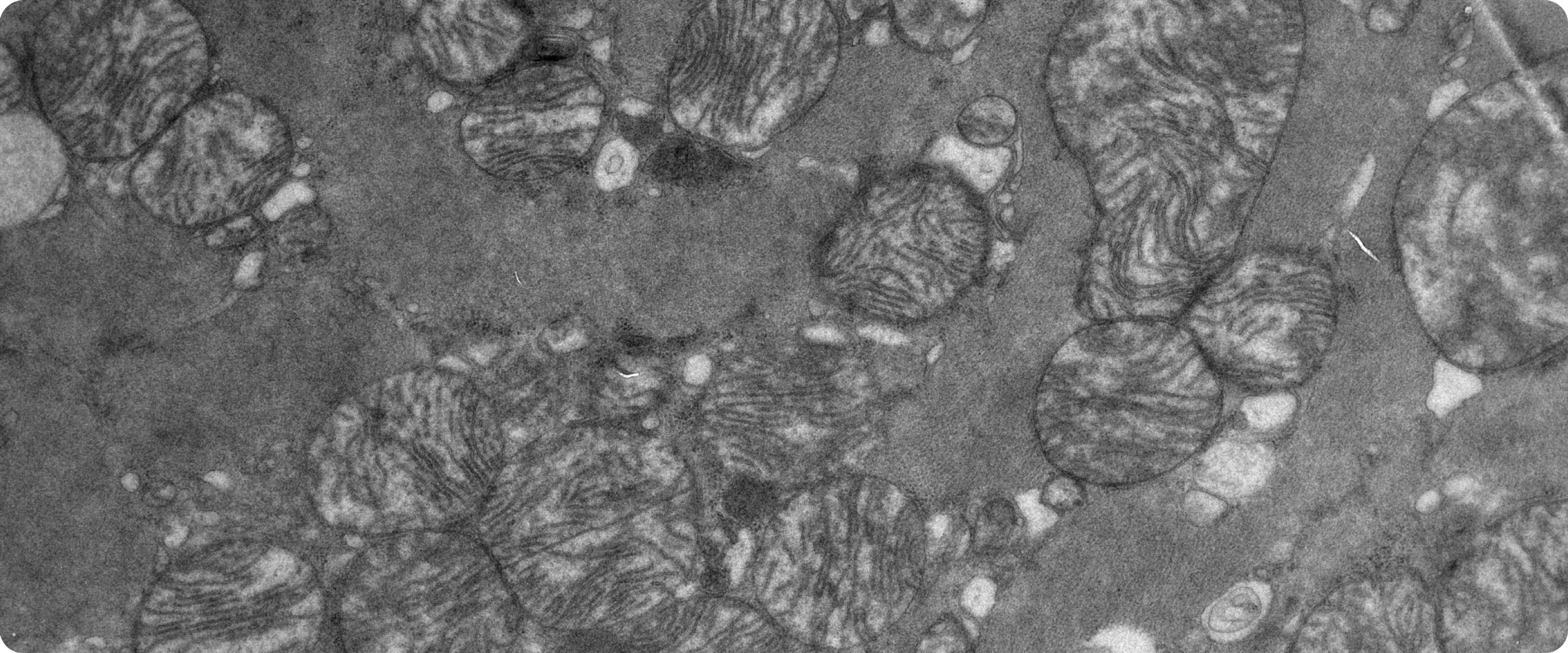
You know that one room in your house that’s off limits to guests? Maybe it’s an office where the valuables are kept. That’s your mitochondria. Your mitochondria are essential components of your cell with various functions, including energy production and playing a central role in the aging process[19].[18]
But mitochondria, especially the fragile DNA inside them, are highly vulnerable to photodamage. When exposed to too much UV light, they become less efficient at generating cellular energy and start producing more harmful free radicals instead.[17]
Normally, mitochondria maintain a delicate balance between generating reactive oxygen species (ROS) and neutralizing them with antioxidants. This balance is critical for supporting skin functions like healing, repair, and regeneration. But repeated UV exposure can disrupt this system, tipping the scale toward oxidative stress.[16]
When cellular energy drops and oxidative damage builds up, essential processes like skin turnover and collagen production slow down. The result: wrinkles, uneven pigmentation, rough texture, and aged skin.
Skin Sensitivity to Photodamage
Our skin’s sensitivity to UV radiation varies dramatically, by more than 100-fold, meaning some individuals are more likely to burn or experience sun damage than others.[20]
The primary determinant is melanin, the pigment that provides natural sun protection by absorbing and neutralizing UV rays. Individuals with deeper skin tones have more melanin and, as a result, greater baseline protection.[21]
However, people of color are still susceptible to photodamage and can develop skin cancers, though their risk is lower than those with lighter skin.[22]
Variations in skin immunity can also shape how different skin types react to UV exposure. Cumulative factors like sunscreen use, pollution, poor diet, smoking, and even lack of exercise, sleep, and stress can weaken the skin’s defenses.[23]
Targeting Photodamage with Urolithin A
The market is flooded with skincare products, promising to slow aging and reverse damage. What if your skincare routine is making your skin more vulnerable to sun damage?
Traditional skincare often asks you to choose: effective or gentle. Many anti-aging ingredients, like retinoids or exfoliating acids, are actives that deliver results by damaging the surface of the skin, forcing cell turnover. Over time, aggressive activities can disturb the intracellular bonds within your skin, leading to flakiness and reduced structural integrity.[27]
Retinoids[24] and alpha-hydroxy acids[25] like glycolic acid[26], have been linked with increased sun sensitivity and likelihood of sunburn and extra precision in the sun is a must.
Sun-damaged skin doesn’t need more stress. It needs cellular-level support that works with your skin, not against it.
This is where the Timeline approach comes in: bioavailable actives that can actually help protect your skin from photodamage, closing the delta between efficacy and tolerance.
Mitopure®: A Superior Active
Our skin line is powered by Mitopure, our highly pure, patented form of Urolithin A, clinically proven to slow key drivers of skin aging when applied topically. Mitopure works at the cellular level, targeting one of the root causes of skin aging: mitochondrial decline.[28]
Mitochondria are the energy powerhouses inside every skin cell. As we age, they get damaged, leading to reduced cellular repair, slower collagen synthesis, and increased inflammation. Mitopure revitalizes these mitochondria, promoting skin health from the inside out.
Slowing Photoaging With Mitopure
Mitopure doesn’t just slow the internal drivers of aging. Clinical trials show that it enhances your healing response to the number one driver of premature skin aging: photodamage.[29]
Enhanced Resilience
Topically applied 1% Mitopure is clinically proven to stimulate collagen-preserving pathways and promote genes associated with collagen organization in the skin.[30]
Lowering Inflammation
Sun-damaged skin (in a Reconstructed Human Epidermis model) treated with 1% Mitopure had significantly reduced levels of PGE2, a molecule associated with skin inflammation. It also inhibits collagen-degrading enzymes (like MMPs).
Reduced Photoaging
Skin treated with 1% Mitopure had a 13% milder sunburn response to UV-B damage, a statistically significant result.
Doesn’t Sensitize
Despite these powerful effects, Mitopure is not a photosensitizer. It does not irritate or weaken the skin barrier. On the contrary, it seems to fortify the skin. [31]That means:
- No need for extra caution during the summer
- Doesn’t have to be reserved for nighttime
- No tedious skin cycling required
- You don’t have to “get used to it” like with retinol
- You don’t have to tolerate peeling, redness, or flaking
Skincare should be productive, not counterproductive. Mitopure helps to keep your routine simple, effective, and most importantly, safe.

Mitopure Firming Serum
4.8 · 1462 reviews
Award-winning bioactive formula for renewal
Photodamaged Prevention: The Best Strategy
Beyond using Mitopure, there are several tried-and-true ways to protect our skin from sun damage. Here are some research-backed strategies.
SPF is non-negotiable. UV damage is cumulative, so daily sun protection is key, even when it’s cloudy or you’re mostly indoors.
Your best bet is a broad-spectrum mineral sunscreen (SPF 30 or higher). Mineral formulas with ingredients like zinc oxide or titanium dioxide physically deflect UV and visible light. They’re especially helpful for sensitive or acne-prone skin.
Dr. Joyce Park, leading board-certified dermatologist, shares the following tip: “If you are mixing your sunscreens with your makeup, your serums, your lotions, or your other skincare products, you are diluting them.”
Apply sunscreen after your skincare dries, and let it form a proper layer on the surface before you put on any makeup.

Antioxidants neutralize the free radicals in your skin. You can bolster your skin’s defenses by eating a healthy diet rich in antioxidant-packed fruits and vegetables (think berries, leafy greens, colorful produce). Vitamins C and E, carotenoids, and polyphenols from foods can all help counter oxidative stress in the body.[33]
Topical products can also contain antioxidants. Studies find that topical application of an antioxidant shield, like that found in Timeline’s Skincare, can reduce the oxidation damage skin suffers from UV exposure.[32]
While topical antioxidants are not a free pass to sunbathe, they do provide supportive protection and can improve photodamage over time.
In addition to a healthy diet, other lifestyle practices can influence skin resilience, including:
- Smoking is a major skin ager. It restricts blood flow, breaks down collagen, and floods your body with free radicals. Quitting can make a visible difference.[34]
- Alcohol dehydrates your skin, dilates blood vessels, and triggers inflammation. It also interferes with nutrient absorption, which is critical for skin repair.[35]
- Sleep is your body’s prime time for recovery. Sleep deprivation disrupts this process, leading to puffiness, dullness, and slower healing.[36]
- Stress also takes a toll. Increases in cortisol, from psychological stress or hormone imbalance, can lead to dryness, irritation, and premature aging.[37]
- Exercise, especially aerobic movement, increases circulation, oxygen delivery, and lymphatic drainage.[38]
The same habits that support your body also build stronger, more resilient skin. And it goes both ways, skin aging isn’t just cosmetic; it influences the pace of overall aging.
Future-Proof Your Skin
Photodamage isn’t just about looks. It’s a cellular-level breakdown that accelerates aging and increases long-term health risks. But now, more than ever, we have the tools to do something about it.
From smart sun protection and antioxidant-rich diets to cutting-edge ingredients like Mitopure, protecting your skin doesn't have to mean choosing between beauty and health, or between results and safety.
It’s time to shift the paradigm: away from harsh actives that stress your skin, and toward solutions that support and strengthen it from within. With a smarter approach to skincare, you can help your skin stay youthful, resilient, and radiant for years to come.
Protect what matters most. Start at the cellular level.
Authors

Written by
Freelance writer

Reviewed by
Director Science Communications
References
- ↑
Ansari, K., Riaz, R., Gull, F., & Atiq, H. (2024). Incorporation of zinc oxide and cobalt doped zinc oxide nano-rods in commercial sunscreen sample to optimize its UV-ray absorption. Physica Scripta, 99. https://doi.org/10.1088/1402-4896/ad5232 (https://www.google.com/url?q=https://doi.org/10.1088/1402-4896/ad5232&sa=D&source=docs&ust=1752161176928738&usg=AOvVaw3ySp8ui692Rd5jM0qC_uRH)
- ↑
Manganelli M, Stabile G, Scharf C, Podo Brunetti A, Paolino G, Giuffrida R, Bigotto GD, Damiano G, Mercuri SR, Sallustio F, et al. Skin Photodamage and Melanomagenesis: A Comprehensive Review. Cancers. 2025; 17(11):1784. https://doi.org/10.3390/cancers17111784 (https://www.google.com/url?q=https://doi.org/10.3390/cancers17111784&sa=D&source=docs&ust=1752161176930668&usg=AOvVaw31DYRjn4CKQT3rvZrpGNdo)
- ↑
Rittié L, Fisher GJ. Natural and sun-induced aging of human skin. Cold Spring Harb Perspect Med. 2015 Jan 5;5(1):a015370. doi: 10.1101/cshperspect.a015370. PMID: 25561721; PMCID: PMC4292080.
- ↑
Kim, H.J., Jin, SP., Kang, J. et al. Uncovering the impact of UV radiation on mitochondria in dermal cells: a STED nanoscopy study. Sci Rep 14, 8675 (2024). https://doi.org/10.1038/s41598-024-55778-z
- ↑
Rittié L, Fisher GJ. Natural and sun-induced aging of human skin. Cold Spring Harb Perspect Med. 2015 Jan 5;5(1):a015370. doi: 10.1101/cshperspect.a015370. PMID: 25561721; PMCID: PMC4292080.
- ↑
"Skin Cancer." American Academy of Dermatology Association, 20 Jun. 2025, www.aad.org/media/stats-skin-cancer (https://www.google.com/url?q=http://www.aad.org/media/stats-skin-cancer&sa=D&source=docs&ust=1752161176929229&usg=AOvVaw11HiZzJ47pFWxyj-Y99-VV). Accessed 30 Jun. 2025.
- ↑
Grant W. B. (2008). The effect of solar UVB doses and vitamin D production, skin cancer action spectra, and smoking in explaining links between skin cancers and solid tumours. European journal of cancer (Oxford, England : 1990), 44(1), 12–15. https://doi.org/10.1016/j.ejca.2007.09.009 (https://doi.org/10.1016/j.ejca.2007.09.009)
- ↑
Griffiths C. E. (1992). The clinical identification and quantification of photodamage. The British journal of dermatology, 127 Suppl 41, 37–42. https://doi.org/10.1111/j.1365-2133.1992.tb16986.x (https://doi.org/10.1111/j.1365-2133.1992.tb16986.x)
- ↑
Griffiths C. E. (1992). The clinical identification and quantification of photodamage. The British journal of dermatology, 127 Suppl 41, 37–42. https://doi.org/10.1111/j.1365-2133.1992.tb16986.x (https://doi.org/10.1111/j.1365-2133.1992.tb16986.x)
- ↑
Griffiths C. E. (1992). The clinical identification and quantification of photodamage. The British journal of dermatology, 127 Suppl 41, 37–42. https://doi.org/10.1111/j.1365-2133.1992.tb16986.x (https://doi.org/10.1111/j.1365-2133.1992.tb16986.x)
- ↑
Shao, Y., Qin, Z., Alexander Wilks, J., Balimunkwe, R. M., Fisher, G. J., Voorhees, J. J., & Quan, T. (2019). Physical properties of the photodamaged human skin dermis: Rougher collagen surface and stiffer/harder mechanical properties. Experimental dermatology, 28(8), 914–921. https://doi.org/10.1111/exd.13728 (https://doi.org/10.1111/exd.13728)
- ↑
Rittié, L., & Fisher, G. J. (2015). Natural and sun-induced aging of human skin. Cold Spring Harbor perspectives in medicine, 5(1), a015370. https://doi.org/10.1101/cshperspect.a015370 (https://doi.org/10.1101/cshperspect.a015370)
- ↑
Del Rosso, J. Q., & Levin, J. (2011). The clinical relevance of maintaining the functional integrity of the stratum corneum in both healthy and disease-affected skin. The Journal of clinical and aesthetic dermatology, 4(9), 22–42.
- ↑
Tabrah F. L. (2010). Human injury from atomic particles and photon exposure: fears, myths, risks, and mortality. Hawaii medical journal, 69(4), 93–98.
- ↑
Tabrah F. L. (2010). Human injury from atomic particles and photon exposure: fears, myths, risks, and mortality. Hawaii medical journal, 69(4), 93–98.
- ↑
Yuan X, Li H, Lee JS, Lee DH. Role of Mitochondrial Dysfunction in UV-Induced Photoaging and Skin Cancers. Exp Dermatol. 2025 May;34(5):e70114. doi: 10.1111/exd.70114. PMID: 40318065.
- ↑
Yuan X, Li H, Lee JS, Lee DH. Role of Mitochondrial Dysfunction in UV-Induced Photoaging and Skin Cancers. Exp Dermatol. 2025 May;34(5):e70114. doi: 10.1111/exd.70114. PMID: 40318065.
- ↑
https://mytohealth.net/wp-content/uploads/2023/05/Pleiotropic-effects-of-mitochondria-in-aging-Nature-Aging-2022.pdf (https://www.google.com/url?q=https://mytohealth.net/wp-content/uploads/2023/05/Pleiotropic-effects-of-mitochondria-in-aging-Nature-Aging-2022.pdf&sa=D&source=docs&ust=1752161176918240&usg=AOvVaw0-JM3Z179Usvak5qgrXdKS)
- ↑
Kim, H.J., Jin, SP., Kang, J. et al. Uncovering the impact of UV radiation on mitochondria in dermal cells: a STED nanoscopy study. Sci Rep 14, 8675 (2024). https://doi.org/10.1038/s41598-024-55778-z
- ↑
Rees J. L. (2004). The genetics of sun sensitivity in humans. American journal of human genetics, 75(5), 739–751. https://doi.org/10.1086/425285 (https://doi.org/10.1086/425285)
- ↑
Rees J. L. (2004). The genetics of sun sensitivity in humans. American journal of human genetics, 75(5), 739–751. https://doi.org/10.1086/425285 (https://doi.org/10.1086/425285)
- ↑
Rees J. L. (2004). The genetics of sun sensitivity in humans. American journal of human genetics, 75(5), 739–751. https://doi.org/10.1086/425285 (https://doi.org/10.1086/425285)
- ↑
Rees J. L. (2004). The genetics of sun sensitivity in humans. American journal of human genetics, 75(5), 739–751. https://doi.org/10.1086/425285 (https://doi.org/10.1086/425285)
- ↑
Tolleson WH, Cherng SH, Xia Q, Boudreau M, Yin JJ, Wamer WG, Howard PC, Yu H, Fu PP. Photodecomposition and phototoxicity of natural retinoids. Int J Environ Res Public Health. 2005 Apr;2(1):147-55. doi: 10.3390/ijerph2005010147. PMID: 16705812; PMCID: PMC3814709.
- ↑
Fiume, M. (2017). Alpha Hydroxy Acids. International Journal of Toxicology, 36, 15S - 21S. https://doi.org/10.1177/1091581817716656 (https://www.google.com/url?q=https://doi.org/10.1177/1091581817716656&sa=D&source=docs&ust=1752161176926702&usg=AOvVaw0Iir9tZlZQzOaVLnClOVe4).
- ↑
The effects of topically applied glycolic acid and salicylic acid on ultraviolet radiation-induced erythema, DNA damage and sunburn cell formation in human skin
Kornhauser, Andrija et al.
Journal of Dermatological Science, Volume 55, Issue 1, 10 - 17 - ↑
Kim, M. Y., Lee, S. E., Chang, J. Y., & Kim, S. C. (2011). Retinoid Induces the Degradation of Corneodesmosomes and Downregulation of Corneodesmosomal Cadherins: Implications on the Mechanism of Retinoid-induced Desquamation. Annals of dermatology, 23(4), 439–447. https://doi.org/10.5021/ad.2011.23.4.439 (https://doi.org/10.5021/ad.2011.23.4.439)
- ↑
Topical application of Urolithin A slows intrinsic skin aging and protects from UVB-mediated photodamage: Findings from Randomized Clinical Trials. D D’Amico, AM Fouassier, J Faitg, N Hennighausen, M Brandt, D Konstantopoulos, C Rinsch, A Singh medRxiv 2023.06.16.23291378; doi: https://doi.org/10.1101/2023.06.16.23291378 (https://www.google.com/url?q=https://doi.org/10.1101/2023.06.16.23291378&sa=D&source=docs&ust=1745857986976886&usg=AOvVaw0Xxu-iuB36mHPYj2yC1vx2)t (https://doi.org/10.1101/2023.06.16.23291378)
- ↑
Topical application of Urolithin A slows intrinsic skin aging and protects from UVB-mediated photodamage: Findings from Randomized Clinical Trials. D D’Amico, AM Fouassier, J Faitg, N Hennighausen, M Brandt, D Konstantopoulos, C Rinsch, A Singh medRxiv 2023.06.16.23291378; doi: https://doi.org/10.1101/2023.06.16.23291378 (https://www.google.com/url?q=https://doi.org/10.1101/2023.06.16.23291378&sa=D&source=docs&ust=1745857986976886&usg=AOvVaw0Xxu-iuB36mHPYj2yC1vx2)t (https://doi.org/10.1101/2023.06.16.23291378)
- ↑
Topical application of Urolithin A slows intrinsic skin aging and protects from UVB-mediated photodamage: Findings from Randomized Clinical Trials. D D’Amico, AM Fouassier, J Faitg, N Hennighausen, M Brandt, D Konstantopoulos, C Rinsch, A Singh medRxiv 2023.06.16.23291378; doi: https://doi.org/10.1101/2023.06.16.23291378 (https://www.google.com/url?q=https://doi.org/10.1101/2023.06.16.23291378&sa=D&source=docs&ust=1745857986976886&usg=AOvVaw0Xxu-iuB36mHPYj2yC1vx2)t (https://doi.org/10.1101/2023.06.16.23291378)
- ↑
Topical application of Urolithin A slows intrinsic skin aging and protects from UVB-mediated photodamage: Findings from Randomized Clinical Trials. D D’Amico, AM Fouassier, J Faitg, N Hennighausen, M Brandt, D Konstantopoulos, C Rinsch, A Singh medRxiv 2023.06.16.23291378; doi: https://doi.org/10.1101/2023.06.16.23291378 (https://www.google.com/url?q=https://doi.org/10.1101/2023.06.16.23291378&sa=D&source=docs&ust=1745857986976886&usg=AOvVaw0Xxu-iuB36mHPYj2yC1vx2)t (https://doi.org/10.1101/2023.06.16.23291378)
- ↑
Addor F. A. S. (2017). Antioxidants in dermatology. Anais brasileiros de dermatologia, 92(3), 356–362. https://doi.org/10.1590/abd1806-4841.20175697 (https://doi.org/10.1590/abd1806-4841.20175697)
- ↑
Addor F. A. S. (2017). Antioxidants in dermatology. Anais brasileiros de dermatologia, 92(3), 356–362. https://doi.org/10.1590/abd1806-4841.20175697 (https://doi.org/10.1590/abd1806-4841.20175697)
- ↑
Goodman, G. D., Kaufman, J., Day, D., Weiss, R., Kawata, A. K., Garcia, J. K., Santangelo, S., & Gallagher, C. J. (2019). Impact of Smoking and Alcohol Use on Facial Aging in Women: Results of a Large Multinational, Multiracial, Cross-sectional Survey. The Journal of clinical and aesthetic dermatology, 12(8), 28–39.
- ↑
Goodman, G. D., Kaufman, J., Day, D., Weiss, R., Kawata, A. K., Garcia, J. K., Santangelo, S., & Gallagher, C. J. (2019). Impact of Smoking and Alcohol Use on Facial Aging in Women: Results of a Large Multinational, Multiracial, Cross-sectional Survey. The Journal of clinical and aesthetic dermatology, 12(8), 28–39.
- ↑
Xerfan, E. M. S., Souza, M. R., Facina, A. S., Tufik, S., & Andersen, M. L. (2025). Can good sleep quality enhance the benefits of oral collagen supplementation in the prevention of skin aging? A brief report. Archives of dermatological research, 317(1), 340. https://doi.org/10.1007/s00403-025-03860-5 (https://doi.org/10.1007/s00403-025-03860-5)
- ↑
Pujos, M., Chamayou-Robert, C., Parat, M., Bonnet, M., Couret, S., Robiolo, A., & Doucet, O. (2025). Impact of Chronic Moderate Psychological Stress on Skin Aging: Exploratory Clinical Study and Cellular Functioning. Journal of cosmetic dermatology, 24(1), e16634. https://doi.org/10.1111/jocd.16634 (https://doi.org/10.1111/jocd.16634)
- ↑
Nishikori, S., Yasuda, J., Murata, K., Takegaki, J., Harada, Y., Shirai, Y., & Fujita, S. (2023). Resistance training rejuvenates aging skin by reducing circulating inflammatory factors and enhancing dermal extracellular matrices. Scientific reports, 13(1), 10214. https://doi.org/10.1038/s41598-023-37207-9 (https://doi.org/10.1038/s41598-023-37207-9)

·
Skincare·
Timeline’s Mitopure® technology is launching globally
·
Skincare·